Melanoma in Skin of Color

What Should I Know About Melanoma in Skin of Color?
First, it’s important to understand that “skin of color” is a term that encompasses many skin tones—from lighter to very dark—and ethnicities—including Asian/Pacific Islander, Black, Hispanic/Latino, American Indian/Alaska Native, and more. This enormous group of people is not a monolith, despite the fact that for the purposes of this webpage we are using one term to describe this group.
Because melanoma is a disease that disproportionately affects non-Hispanic Whites (typically those of European descent), most of the data available is, understandably, from patients who are non-Hispanic Whites. But people with skin of color do develop melanoma, and more data is emerging to better understand melanoma in this population. This section of our website addresses the question: How does melanoma affect those with Skin of Color? The answers will be somewhat different for different ethnicities and skin tones.
What is Melanoma?
Melanoma is a type of skin cancer that occurs when pigment-producing cells—known as melanocytes—mutate and become cancerous. Melanocytes, along with basal cells and squamous cells, are the building blocks of human skin, and these cells reside in the top layer of our skin, called the epidermis. Any of these cellular building blocks can grow erratically and out of control and become cancerous. If melanocytes are the cell type that becomes cancerous, we call it melanoma.
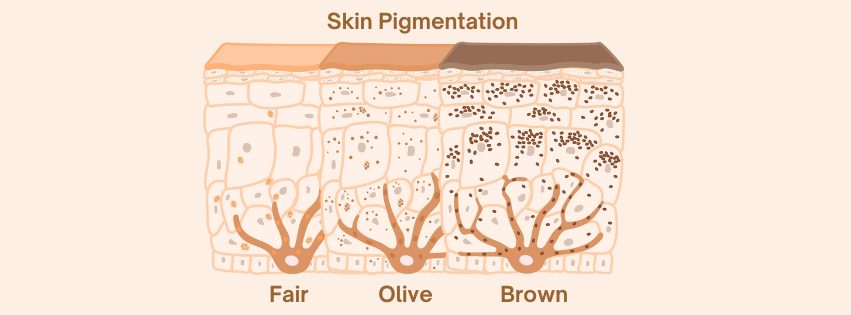
The normal function of a melanocyte is to produce and secrete melanin pigments to give to the surrounding skin cells. The skin cells will engulf, or swallow, the melanin, and this process provides skin with coloration. No matter what your skin tone is, we all have roughly the same number of melanocytes within our skin, but the darker your skin is, the more melanin those melanocytes have produced. Lots of melanin creates dark, brown-black colored skin, and a lack of melanin leaves skin light-colored, or “white.” Since melanin pigment provides a layer of protection for our skin cells against ultraviolet radiation (UV), more color gives some protection against the sun’s harmful rays.
Melanocytes also exist in the mucous membranes, or moist surfaces, of areas inside your body. These mucous membranes line areas such as the sinuses, nasal passages, oral cavity, vagina, and anus. Like the melanocytes found in the skin, mucosal melanocytes can mutate and become cancerous. These changes result in the development of a type of melanoma called mucosal melanoma.
Who Develops Melanoma?
Although it is relatively rare for non-Hispanic Black, Asian/Pacific Islanders or Hispanic individuals to develop melanoma, no one is immune to this disease.1 Melanoma is more likely to occur among those with less melanin and therefore lighter complexions, but it can develop in people with all skin tones.
American Indian/Alaska Natives have the second-highest incidence of melanoma diagnosed in the U.S.2 In fact, the rate of American Indian/Alaska Native males receiving a diagnosis of melanoma doubled between 2011 -2021.3 The incidence of late-stage melanoma diagnoses—meaning the disease is diagnosed when it has already spread—is also rising in American Indian/Alaska Natives.4
For the Hispanic population residing in the U.S., which includes Mexican, Puerto Rican, Spanish, Salvadoran, Cuban, Dominican, Guatemalan, and other ethnic groups, the rate of melanoma is low, but it is increasing. Between 2000 to 2021, each year the percentage of Hispanic people diagnosed with melanoma grew by 0.4%.3 While this may seem like a small increment, over time it has led to a significant increase in the rate of melanoma in this population, which mainly resides in the Southwestern regions of the U.S. that have high levels of UV radiation.5
For every 100,000 individuals in the U.S., how many men will be diagnosed with melanoma?4
- American Indian/Alaska Natives – 17.4
- Asian American/Pacific Islander – 1.4
- Black – 0.8
- Hispanic – 4.8
- White, non-Hispanic – 40.3
For every 100,000 individuals in the U.S., how many women will be diagnosed with melanoma?4
- American Indian/Alaska Natives – 7.5
- Asian American/Pacific Islander – 1.2
- Black – 1.1
- Hispanic – 4.9
- White, non-Hispanic – 27.9
As you can see in the statistics above, only about one in 100,000 Black men will develop melanoma—it’s a rare disease for Black men. Over 17 in 100,000 American Indian/Alaska Native men will develop melanoma, a rate which is substantially higher than other men and women with skin of color. Bottom line: Melanoma does occur in people with skin of color, so it’s important to be aware of the disease, even if it is rare. Additionally, many of us are a mix of heritages, so our risk may not be easily calculated.
What are Some Differences in Melanoma Outcomes, Stages, and Subtypes?
Being aware of melanoma can save lives. How? Because early-stage melanoma is more treatable and survivable than later stage melanoma. Generally, melanoma that is detected early, before it has spread (Stage I and II), has a very high survival rate. But the survival rate of melanoma that is detected after it has spread (Stage III and IV) is significantly lower. Awareness of the disease can lead to early detection, which can save lives. >>Learn about the stages of melanoma (click for more information)
Differences in Outcomes
Because skin cancer is not a common cancer in people of color, there is often a lack of community awareness of the disease—including how to prevent it and what to look for on your skin. Additionally, there is a misconception that melanoma only occurs in sun-exposed areas. Finally, the medical community may lack suspicion or awareness of how skin cancer presents in skin of color. All of these circumstances lead to skin cancer being diagnosed in people with skin of color at a more advanced stage and when it is harder to treat, which contributes to disparities in outcomes of care. For example, only 65% of melanomas are found among Hispanic individuals at a localized, early stage, compared to 78% among White individuals.5 This difference corresponds to a disparity in the 5-year survival rate for Hispanic patients diagnosed with melanoma, which was 83% versus 94% for White patients for all stages of the disease.5
Another study demonstrated a striking disparity between White and Black individuals related to when their disease was first detected: 39% of Black patients presented with regional or distant melanoma (Stage III or Stage IV) while only 15% of White patients presented at these later stages.6 In the same study, looking at patients diagnosed with localized melanoma (Stage I and II), patients with skin of color were more likely to have ulcerated melanomas—meaning the skin over the melanoma is not intact—and significantly thicker melanomas. Ulceration and thicker melanomas are usually associated with worse outcomes.
In people with skin of color, even localized melanoma (melanoma that has not spread; Stage I or II) is more deadly than for White non-Hispanics (see statistics below).
Five-Year Relative Survival of Localized Cutaneous Melanoma (2014-2020) 7
- American Indian/Alaska Natives – 92%
- Asian American/Pacific Islander – 93%
- Black – 89%
- Hispanic – 96%
- White, non-Hispanic – 99%
Another striking outcome-related example concerns Asian American/Pacific Islanders’ melanoma mortality rates: For advanced-stage melanoma, the 5-year survival rate between 2014-2020 was the lowest for Asian American/Pacific Islanders (22%) in comparison to all other ethnicities (ranging between 23-36%).7 So despite having a comparatively low risk for melanoma, Asian Americans are more likely to die from late-stage melanoma than all other ethnicities. We need more research to understand why advanced-stage melanoma is so lethal to a specific ethnicity, especially one that is the fastest growing racial/ethnic population in the U.S.8
All of these disparities are concerning and point to the critical need for melanoma awareness, education about early detection, and research in people with skin of color.
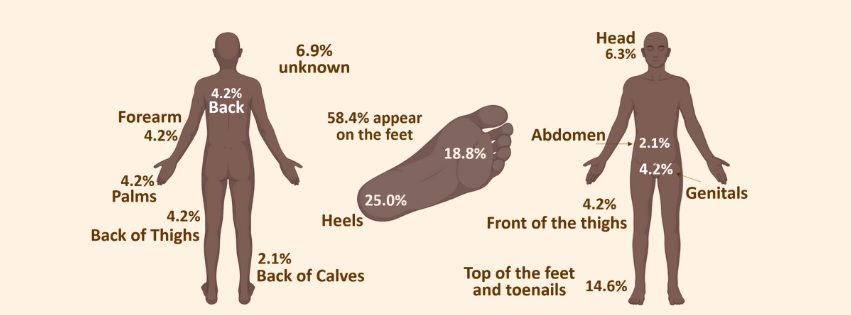
Differences in Location of Melanoma
There are also major differences in the location of primary melanomas between ethnic heritages, races, and sexes. For example, in a study of Black patients, the primary tumor spot most commonly diagnosed was on the bottom of the feet, a site usually considered to be exclusive to a subtype of melanoma called acral lentiginous melanoma (see more information on subtypes, below).9 In Asian American individuals, melanoma is often diagnosed on the lower extremities.8 In American Indian/Alaska Native women, melanoma is often found on the lower limb or hip. Among American Indian/Alaska Native men, melanoma is often detected on the ear, face, neck, scalp, shoulders, or upper limbs.2
Differences in Subtypes of Melanoma
Different ethnic heritages and races also see differences in melanoma subtypes. The subtype acral lentiginous melanoma accounts for over 17% of melanomas diagnosed in non-Hispanic Blacks, over 19% in Hispanic non-Whites, over 11% in non-Hispanic Asian/Pacific Islanders, but only 0.8% in non-Hispanic Whites.10 A higher percentage of patients with skin of color are diagnosed with mucosal melanoma—the type found on mucosal surfaces such as inside your anus, mouth, or vagina.
While the overall incidence of melanoma is lower in people with skin of color, it is critical that we improve community awareness and awareness in the medical profession, in order to improve prevention and timely identification of the disease. Early detection will save lives.
References
1. Brunsgaard EK, Jensen J, Grossman D. Melanoma in skin of color: Part II. Racial disparities, role of UV, and interventions for earlier detection. J Am Acad Dermatol. 2023;89(3):459-468. doi: 10.1016/j.jaad.2022.04.057.
2. Townsend JS, Melkonian SC, Jim MA, et al. Melanoma Incidence Rates Among Non-Hispanic American Indian/Alaska Native Individuals, 1999-2019. JAMA Dermatol. 2023;e235226. doi: 10.1001/jamadermatol.2023.5226.
3. SEER*Explorer: An interactive website for SEER cancer statistics. Surveillance Research Program, National Cancer Institute; 2024 Apr 17. Updated 11.5.2024. Accessed 2.7.2025. Available from: https://seer.cancer.gov/statistics-network/explorer/.
4. Kohn LL, Zullo SW, Manson SM. High Melanoma Rates in the American Indian and Alaska Native Population—A Unique Challenge. JAMA Dermatol. 2024;160(2):145-147. doi:10.1001/jamadermatol.2023.5225.
5. American Cancer Society. Cancer Facts & Figures for Hispanic/Latino People 2024-2026. Atlanta: American Cancer Society; 2024.
6. American Cancer Society, 2025. Cancer Statistics Center. Survival data adjusted for normal life expectancy and cases from 2014-2020. Updated 2024. Accessed 2.7.2025. Available at https://cancerstatisticscenter.cancer.org/#/
7. American Cancer Society. Cancer Facts & Figures for Asian American, Native Hawaiian, & Other Pacific Islander People 2024-2026. Atlanta: American Cancer Society; 2024.
8. Kim DY, Dee EC, Cheng I et al. Advanced melanoma presentation and disease-specific survival disparities among disaggregated Asian American, Native Hawaiian, and Pacific Islander populations. J Am Acad Dermatol. 2024;90(3):623-626. doi: 10.1016/j.jaad.2023.10.052.
9. Wix SN, Brown AB, Heberton M et al. Clinical Features and Outcomes of Black Patients With Melanoma. JAMA Dermatol. 2024;160(3):328-333. doi: 10.1001/jamadermatol.2023.5789
10. Holman DM, King JB, White A et al. Acral lentiginous melanoma incidence by sex, race, ethnicity, and stage in the United States, 2010–2019. Prev Med. 2023:175:107692. doi: 10.1016/j.ypmed.2023.107692.

