Side Effect Central: Lichen Planus Explained

Side Effect Central is a new series of articles designed to help patients with melanoma and their caregivers understand the side effects that typically accompany melanoma treatments. Our goal is to explain what side effects to expect during treatment and to encourage communication with your medical team about these side effects.
Side effects can range from mild to very serious, and doctors cannot predict who will suffer more side effects than others. Serious side effects can cause patients to interrupt or discontinue treatment, and they can lead to dangerous and possibly deadly consequences, so managing them is a critical piece of melanoma treatment.
While many people expect fatigue or nausea during melanoma treatment, some side effects are more unexpected—and just as disruptive. One of these is lichen planus, a condition that can affect the skin or oral cavities. It’s important for patients and caregivers to recognize the signs early and understand how it can be managed.
What is Lichen planus?
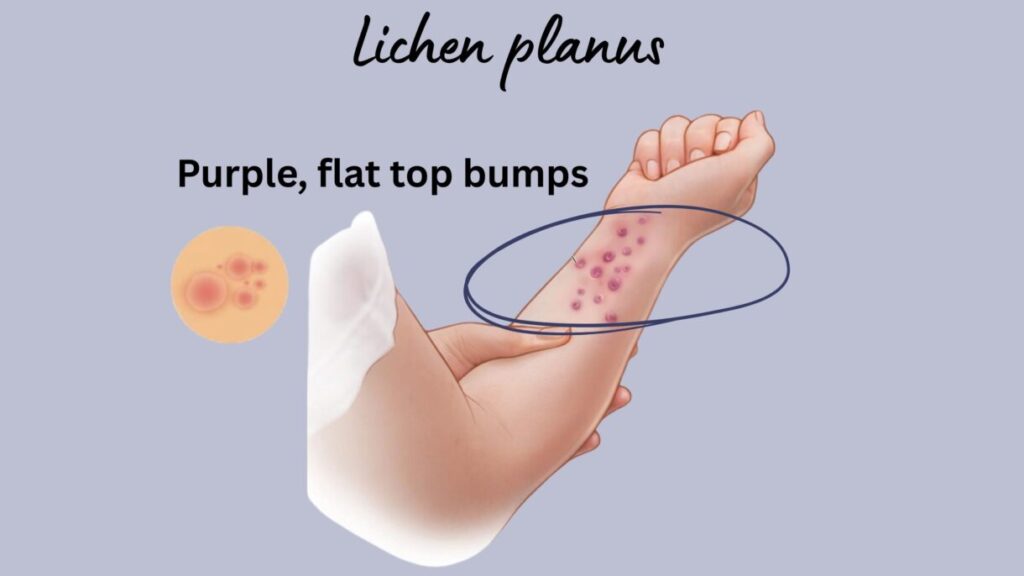
Lichen planus is an inflammatory skin condition that causes a skin rash with dark red or purple bumps that have a flat top. The bumps are usually small, starting the size of a pin and increasing to <1 cm. They are associated with a severe itching sensation.
The bumps may start out looking light pink in color and emerge on the skin of the ankles, back of the hands, elbows, lower back, lower legs, truck or wrists. Sometimes lichen planus affects the oral cavity, nails, and genitals. Here, we will focus more on the skin, not as much on the oral condition associated with lichen planus, which can present differently.
Lichen planus occurs in <1% of the adult population over 40 years of age, but up to 6% of patients who are receiving immune checkpoint inhibitors, such as ipilimumab (Yervoy), nivolumab (Opdivo), and pembrolizumab (Keytruda). For the small percentage of patients who develop these rashes, they usually appear six to twelve weeks after beginning immune checkpoint inhibitor therapy.
What should patients know?
Although skin rashes and intense itching can become an uncomfortable and unbearable distraction, rarely does it become potentially life-threatening. If possible, it is best to avoid scratching the area to prevent opening the skin, which could lead to an infection.
Many patients may be able to stay on their drug regimens for melanoma when a mild or moderate inflammation of the skin occurs. However, there are long-term consequences of inattention, so seeking treatment is important. Patients should promptly communicate with their health care team and seek treatment when observing any of the symptoms listed below.
Mild to moderate symptoms—report to your health care team
- Rash covering <30% of the body that has either small pink or flat red/purple bumps
- Severe itching around or on the rash
- Sores in your mouth or genital area that look white in color
Serious symptoms—report to your health care team
- Rash covering >30% of the body with flat red/purple bumps
- Intense itching that interferes with your daily activities, like sleep
- Peeling skin that is sloughing off your body
- Blisters in your mouth or genital area
Long-term consequences of avoiding treatment
- A small percentage of oral lichen planus and oral lesions (0.5-2.5%) undergo malignant transformations to oral cutaneous squamous cell carcinoma within five years. All patients with this complication of immune checkpoint inhibitors should be monitored by their dental practitioner and/or general health clinician for this occurrence.
Why does lichen planus occur?
Immunotherapy is designed to supercharge the immune system. In the case of immune checkpoint inhibitors, these remove the brakes put on immune cells by cancer cells. When the brakes are removed, the immune system becomes activated.
Unfortunately, the skin can become susceptible to an immune system-provoked injury as an unintended consequence. Although immunotherapy is created with targeted properties aimed at the tumor’s environment, sometimes it non-specifically activates too much of the immune system throughout the body.
Nearly every organ system in the body is at risk for an unprovoked injury by immune checkpoint inhibitors. However, immunotherapy works so well in many patients that the risk of side effects is deemed worthwhile to achieve the possible results. Prompt and thorough communication about side effects by patients with their medical team allows for appropriate clinical support, and these two together allow immunotherapy to be used safely and successfully in many patients. Individual perspectives about treatment ideals should be discussed with your clinician.
What can a clinician do to treat lichen planus associated skin rash and itching?
Rapid identification and treatment can reduce the discomfort induced from mild itching. Early management of this side effect can avoid drug interruption or discontinuation and allow a patient to remain on therapy. Once a definitive diagnosis is made, the treatment depends on how much (%) of the body surface is covered in the rash.
For example, if <10% of the skin has a rash, it is considered a mild condition. Immunotherapy will not be withheld from the patient. For relief, a topical steroid like clobestasol 0.05%, fluocinonide 0.05%, or tacrolimus 0.1% ointment could be prescribed for application.
If more that 30% of the skin has a rash, then the condition is severe. Immunotherapy will be withheld. In addition to the treatments given for a mild condition, oral steroids like prednisone or intravenous methylprednisolone may be prescribed. A clinician could also refer the patient to a dermatologist who may consider acitretin, doxycycline, nicotinamide, or other drugs.
Bottom line: Patients should communicate regularly with their medical team about any of the signs of a skin rash and itching, as noted above. Clinicians can then manage and treat the condition to allow the patient to remain on immunotherapy or resume treatment as quickly as possible.
References:
Binnie R, Dobson ML, Chrystal A et al. Oral lichen planus and lichenoid lesions – challenges and pitfalls for the general dental practitioner. Br Dent J. 2024;236(4):285-292. doi: 10.1038/s41415-024-7063-y.
Thompson JA, Schneider BJ, Brahmer J et al. Management of Immunotherapy-Related Toxicities, Version 2.2024. Featured Updates to the NCCN Guidelines. J Natl Compr Canc Netw. 2024;22(9):582-592. doi: 10.6004/jnccn.2024.0057.
Recent Posts

Update on the State of Vaccines for Melanoma

Healing Through Creativity: Art Therapy in Cancer Care

Side Effect Central: Lichen Planus Explained

Behavioral Addiction Responsible for Excessive Indoor Tanning


