Leptomeningeal Metastasis
What is leptomeningeal metastasis?
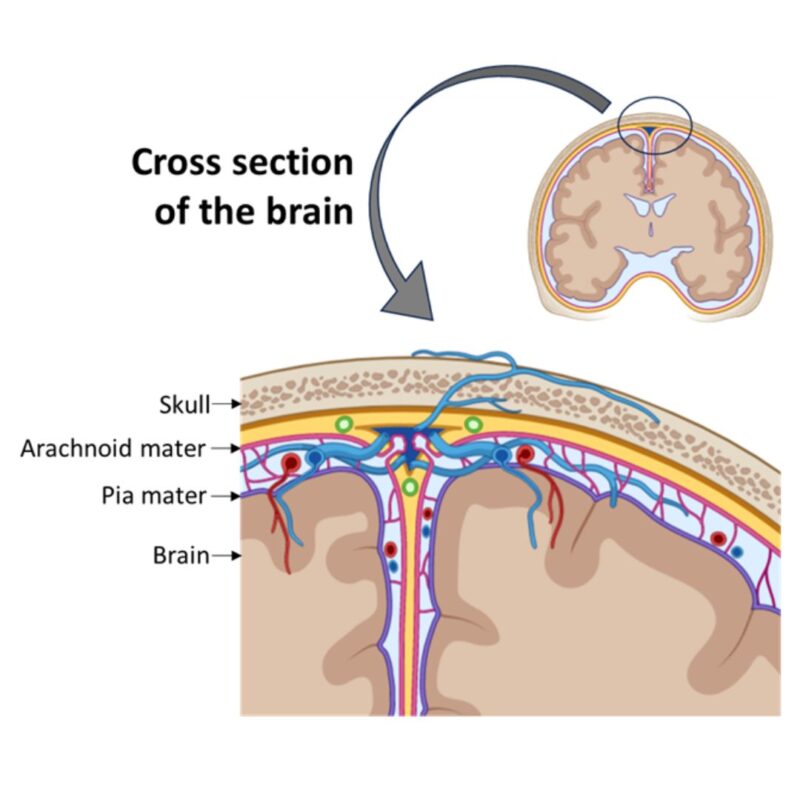
Leptomeningeal metastasis—also called leptomeningeal carcinomatosis, leptomeningeal disease, or simply “LMD”—is the spread of cancer to a particular part of the brain called the leptomeninges. It is different from brain metastases occurring inside the “meat” of your brain, because LMD grows in the lining of the brain, the leptomeninges. It is a complication that can arise from numerous cancers, but unfortunately not uncommon in metastatic (Stage IV) melanoma.
LMD is named after the structures of the brain, the leptomeninges. Together the leptomeninges comprise different layers which include the arachnoid mater and pia mater, with a space between them. The arachnoid mater and pia mater are two thin, delicate membranes covering the brain and spinal cord. When the cancer cells settle and grow in this area, we call this LMD.
Many solid tumors can produce leptomeningeal metastases, with the most common ones being melanoma, breast cancer, and lung cancer. Among patients diagnosed with metastatic melanoma, 10-15% will develop leptomeningeal metastasis, most often later in their cancer journey.
Symptoms
The symptoms of LMD vary greatly in each patient, but can include headaches, cognitive impairment and confusion, seizures, dysfunction of the bladder and bowel, double vision or hearing loss, difficulty walking, back pain, and loss of some nerve function. Sometimes, changes in mental function are first noticed by people closest to the sufferer. Many of these symptoms manifest due to increased pressure in the brain or the nerves being directly affected.
Diagnosis
Often, various tests are needed to definitely confirm a diagnosis of LMD, which can be very challenging due to the location of the cancer and how it is growing. While an MRI or the brain and/or spine by itself can lead to the diagnosis, other techniques may be required to help assess whether you have leptomeningeal metastasis. This can include a lumbar puncture which samples your cerebrospinal fluid (CSF) for cancer cells.
For diagnosing LMD, the “gold standard” is the observation of cancer cells in CSF because a pathologist can get a microscopic view of the cells and determine whether they are cancerous. Please note that sometimes repeated lumbar puncture/CSF analysis is necessary, as the ability to detect cancer cells within the CSF increases with subsequent collections from lumbar puncture.
Another option to confirm diagnosis is the use of liquid biopsies for cell-free DNA evaluation; however, this test is still not broadly used for the diagnosis of LMD. This test may show tumor-specific mutations (which confirm melanoma metastasis in the leptomeninges) to support a diagnosis. Combining results from these various techniques can lead to the diagnosis of leptomeningeal metastasis.
Treatment
If you are diagnosed with leptomeningeal metastasis, the goals of treatment will include maximizing the quality of your life and prolonging survival. Current therapies primarily seek an improvement in neurologic symptoms. Although the prognosis for patients with leptomeningeal metastasis is challenging, treatment can potentially double the life expectancy for patients with this disease. There is no cure for leptomeningeal metastasis, but clinical trials are ongoing to improve the outcomes of patients with LMD.
Palliative therapy and strategies to mitigate symptoms are therefore used in patients with leptomeningeal metastasis. Palliation for pain control using opioids or non-opioids, and using antiseizure medication, antidepressants or psychostimulants may be warranted. Radiation therapy to the whole brain and/or parts of the spine may also be done to alleviate pain and minimize the burden of neurological symptoms. Palliation and radiation therapy are performed for comfort, without intending to increase survival time.
Surgery is rarely used in the treatment of LMD. Your doctor might recommend in special circumstances to administrate treatment directly into your spinal cord, called “intrathecal injection”, and a port called “Ommaya” is installed. This can be used to either instill immunotherapy or chemotherapy into your CSF.
Your doctor might also recommend medication to continue to fight the cancer cells in this part of the brain, but your results will depend upon whether you had prior exposure to those drugs. Immunotherapies nivolumab (OPDIVO®), pembrolizumab (Keytruda®), and ipilimumab (Yervoy®) have shown a very limited benefit in patients with leptomeningeal metastasis. Targeted therapy such dabrafenib (Tafinlar®) and trametinib (Mekinist®) or encorafenib (Braftovi®) and binimetinib (Mektovi®) may also be considered, depending on the advice of the provider and the gene mutation expressed by your tumor. In rare cases, your doctor might also recommend the chemotherapy pill called temozolomide (Temodar®).
Sources:
Batool A, Kasi A. Leptomeningeal Carcinomatosis. [Updated 2023 Mar 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
Steininger J, Gellrich FF, Engellandt K, et al. Leptomeningeal Metastases in Melanoma Patients: An Update on and Future Perspectives for Diagnosis and Treatment. Int J Mol Sci. 2023;24(14):11443. doi: 10.3390/ijms241411443.

