Cutaneous Melanoma
What is Cutaneous Melanoma?
Cutaneous Melanoma
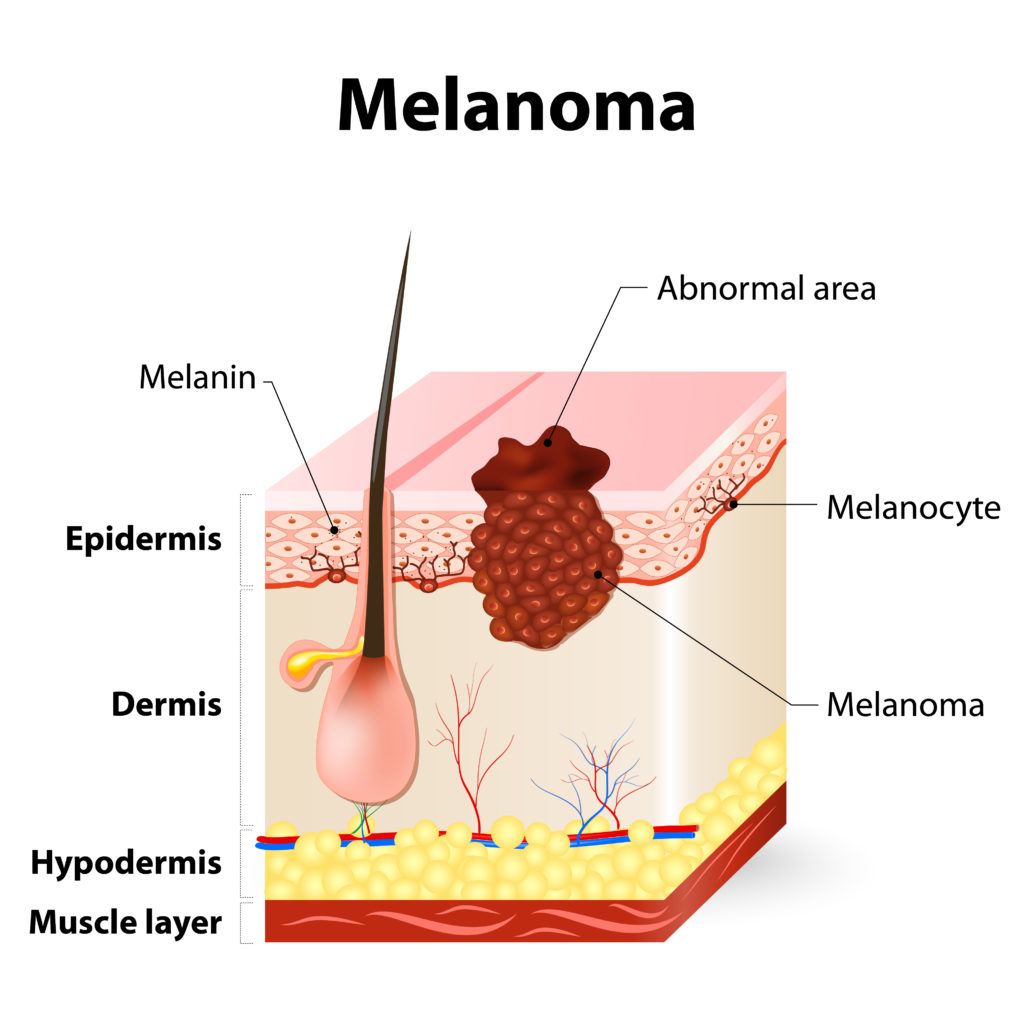
Cutaneous or skin melanoma (also called malignant melanoma, although any diagnosis of melanoma is cancer even if “malignant” is not used) develops in pigment cells called melanocytes. These melanocytes produce melanin, the vital pigment that gives our skin its color and protects it from damage caused by ultraviolet (UV) rays from the sun or tanning devices. Cutaneous melanoma occurs when cancerous cells grow out of control (mutate) and crowd out normal cells. Usually, cutaneous melanoma begins in the epidermis—the top layer of skin—and can become invasive from there.
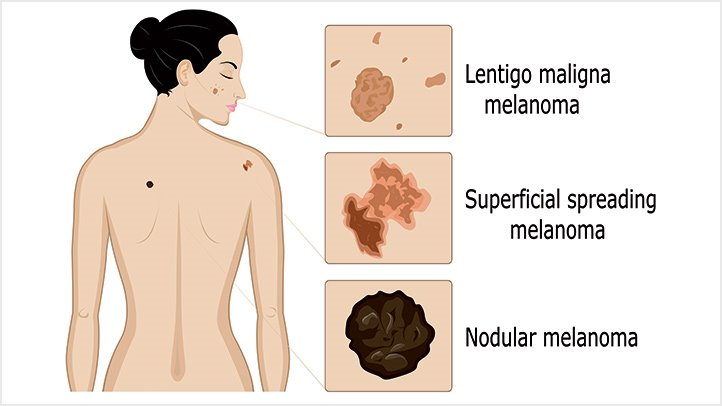
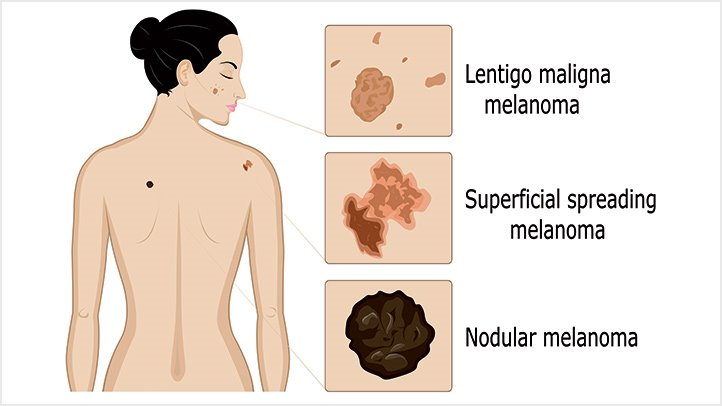
There are four main subtypes of cutaneous melanoma: superficial spreading melanoma; nodular melanoma; lentigo maligna melanoma; and acral lentiginous melanoma (ALM). Other subtypes, such as desmoplastic and amelanotic melanoma, also exist but are rare.
Superficial Spreading Melanoma
What It Is: The most common type of melanoma, representing about 70% of all cases. It begins in the melanocytes and spreads on the surface of the skin (“superficial”) before it grows deeper and becomes invasive. This type of melanoma usually appears as a flat or barely raised lesion on the surface of the skin, often with irregular borders and variations in color. About half of these melanomas occur in pre-existing moles; the other half occur in new lesions.[1] These lesions most commonly appear on the trunks of men, the legs of women, and the upper back of both sexes. This type of melanoma is diagnosed most frequently in patients between the ages of 30 and 50.
How It Progresses: It spreads along the top layer of skin—the epidermis—for a period of months to years before it goes deeper into the skin.
Signs: The darkening in one part of a pre-existing mole or the appearance of a new mole on unaffected, normal skin.
Nodular Melanoma
What It Is: Nodular melanoma is the second most common subtype of superficial spreading melanoma as well as the most aggressive form of the disease. It accounts for 10% to 15% of all cases of melanoma. Nodular melanoma usually appears on the trunk, head or neck and is more common in men than women.
How It Progresses: Unlike other melanomas that tend to grow across the surface of the skin (like an oil slick spreading), a nodular melanoma invades more deeply earlier and therefore often presents with a greater depth of invasion when it is found and biopsied. For this reason, nodular melanomas are more frequently associated with a poorer prognosis than other melanomas.
Signs: This melanoma usually appears as a blue-black, dome-shaped nodule, although 5% of the time the lesions are pink or red.
Lentigo Maligna Melanoma
What It Is: This melanoma comes from a preexisting lentigo, rather than a mole. A lentigo is a dark, flat or slightly raised, non-cancerous spot on the skin, also known as a sunspot. Historically, only about 5% of all melanoma cases are lentigo maligna melanoma.
How It Progresses: This type of melanoma typically takes many years to develop. It is most often found in elderly adults and on parts of the body that have been overexposed to the sun, such as the face, ears, arms, chest, and back. The rate of lentigo maligna melanoma has been steadily increasing over the last few decades. This increase is thought to be due to the fact that the development of lentigo maligna melanoma is influenced by chronic sun exposure.[2]
Signs: Like superficial spreading melanoma, lentigo maligna melanoma usually grows slowly across the top layer of skin and generally appears as a large, slightly-raised patch containing differing shades of color.
Acral Lentiginous Melanoma
What It Is: “Acral” comes from the Greek word akron, meaning extremity, and this fourth type of skin melanoma typically appears on the palms, on the soles, or under the nails. Acral lentiginous melanoma (ALM) can be difficult to diagnosis and has a lower response rate to available therapies for cutaneous melanoma, such as immune checkpoint inhibitors, but survival in the metastatic setting is second only to pure cutaneous melanoma. Less than 5% of all melanomas are ALM, but it is the most common form of melanoma in people with darker skin and those of Asian descent.
How It Progresses: Like superficial spreading melanoma, ALM grows on the surface of the skin or under the nail bed before becoming invasive. Because of the misconceptions that melanomas only occur in sun-exposed areas and that people of color are not at risk for melanoma, these melanomas can be discovered later than other types, after they have invaded deeper layers of skin or metastasized.
Signs: When ALM appears on the palm or sole, it looks like a bruise or an elevated, thickened patch—usually tan, brown, or black, with variations in color and irregular borders. When ALM occurs under the fingernail or toenail, it may present as a brown, black, or blue streak in the nail. In darkly pigmented individuals, it can be completely normal to have darker streaks under the nail because of the increased amount of melanin that their normal melanocytes produce. However, in a lightly pigmented person, dark streaks in the nail are very rare, and any streak that cannot be explained by a trauma must be seriously considered for a biopsy to prove that there is no cancer under the nail.

Amelanotic Melanoma
What it is: Amelanotic melanoma (AM) is a rare type of cutaneous melanoma, representing about 4% of cases. AM is defined by its lack of color, or lack of pigment although a substantial subset of amelanotic melanomas is red or pink. The subtypes listed above can be amelanotic. Although Amelanotic melanoma can occur on all body sites, it is more common on chronically sun-exposed areas.
How it progresses: AM can progress in a variety of ways. It is often diagnosed at a later stage than pigmented melanomas.
Signs: AM doesn’t contain melanin, so it does not look like a mole or appear like a mole. An amelanotic melanoma may be a faint reddish or pinkish color or it may have no color at all; it may an area of skin that simply looks different from that around it.
Desmoplastic Melanoma
What it is: Desmoplastic melanoma (DM) is a rare type of melanoma, representing less than 4% of cases. It can occur on its own or in conjunction with another subtype of melanoma. It can be labeled as “pure” or “mixed” desmoplastic melanoma. Its development is related to chronic UV exposure and is often found on head and neck, trunk, or extremities of older individuals.
How it progresses: DM is challenging because it presents and progresses in a variety of different ways.
Signs: Desmoplastic melanoma can present in a number of ways, so it’s difficult to describe what to look for. However, it is often non-pigmented, and it may present as an amelanotic scar-like or thickened lesion.
Amelanotic Melanoma
What it is: Amelanotic melanoma (AM) is a rare type of cutaneous melanoma, representing about 4% of cases. AM is defined by its lack of color, or lack of pigment although a substantial subset of amelanotic melanomas is red or pink. The subtypes listed above can be amelanotic. Although Amelanotic melanoma can occur on all body sites, it is more common on chronically sun-exposed areas.
How it progresses: AM can progress in a variety of ways. It is often diagnosed at a later stage than pigmented melanomas.
Signs: AM doesn’t contain melanin, so it does not look like a mole or appear like a mole. An amelanotic melanoma may be a faint reddish or pinkish color or it may have no color at all; it may an area of skin that simply looks different from that around it.
Desmoplastic Melanoma
What it is: Desmoplastic melanoma (DM) is a rare type of melanoma, representing less than 4% of cases. It can occur on its own or in conjunction with another subtype of melanoma. It can be labeled as “pure” or “mixed” desmoplastic melanoma. Its development is related to chronic UV exposure and is often found on head and neck, trunk, or extremities of older individuals.
How it progresses: DM is challenging because it presents and progresses in a variety of different ways.
Signs: Desmoplastic melanoma can present in a number of ways, so it’s difficult to describe what to look for. However, it is often non-pigmented, and it may present as an amelanotic scar-like or thickened lesion.
References
J Am Acad Dermatol. 2019 May;80(5):1292-1298. doi: 10.1016/j.jaad.2019.01.012. Epub 2019 Jan 14.

